33rd Annual Congress – DIGITAL

 LIVES, 06-09 December 2020, DIGITAL
LIVES, 06-09 December 2020, DIGITAL
LIVES 2020 will be our first entirely virtual and digital event, and as diverse and stimulating as the face-to-face congress.
We have prepared an outstanding programme of exceptional science that is both interactive, innovative and informative, while connecting our multidisciplinary network of physicians, researchers, nurses, and allied health professionals across the globe.
Our 7 broadcasting channels will offer a live programme of interactive debates, demonstration events, and dynamic presentations/discussions.
We will also provide a wide range of on-demand videos, available to participants on our digital platform from Sunday 6 December at 14:30 CET. The sessions featured in the video on demand programme have no set schedule nor Q&A. This will give delegates the flexibility to watch all the lectures at a time that suits them.
If you have registered for the congress, you should have received an email with information on how to access the congress, complete with URL and login details.
GENERAL INFORMATION
LIVES is going digital!
 General Information
General Information
LIVES IS GOING DIGITAL! 06-09 DECEMBER 2020
Given the continuing impact of the SARS-CoV-2 pandemic, including resulting travel restrictions, ESICM has decided to transition the onsite LIVES 2020 congress to an immersive and exciting online event - LIVES Digital 2020 - from 06–09 December 2020.
ESICM has been live-streaming sessions at its events since 2014 and providing educational content online through the ESICM media library, e-LIVES. Our first-hand experience of delivering online content to the Intensive Care community will now be stepped up to the next level, at LIVES Digital 2020.
LIVES Digital 2020 will be an innovative and engaging digital event for the global intensive care community.
Our carefully-selected scientific content will be live and on-demand, with an exciting digital Congress Programme that will offer unprecedented global relevance and reach, as well as maximum convenience. Wherever you are working or residing and whatever the time, all the key presentations (and more) will be available to you at the click of a key.
The event will come to you from the ESICM online platform and we have developed a host of networking and interactive opportunities, as well as a LIVES Digital central area, where you can connect with the ESICM leadership and staff.
Our aim to is to offer you a LIVES Digital 2020 experience as diverse and stimulating as the face-to-face meeting.
We look forward to meeting you online in December. In the meantime, we would like to use this opportunity to give recognition to the tremendous healthcare professionals throughout the world who are caring for so many patients during this pandemic.
Together we are Intensive Care.
What does this mean?
Instead of us meeting at a physical location this year for our annual congress, which had been previously planned for Madrid, we will now hold the congress completely virtually and online. No travel, fewer obstacles, and more opportunities.
Save the date!
The congress dates will be 06-09 December 2020. More information will be coming in the next weeks as we continue to work on making this as smooth a transition as possible for our entire community. We thank you for your patience and understanding as we first work out the complexities of moving from a physical congress to an online event.
We invite you to visit our websites regularly for the most up-to-date information on the congress and other ESICM activities.
Frequently Asked Questions
 Still have questions? See our FAQ below.
Still have questions? See our FAQ below.
Links and all necessary information on how to access LIVES online will be emailed to you on Saturday 5 December.
You will be able to review the sessions and visit the virtual exhibition via the link sent to you (i.e., from the virtual platform) throughout the 6 months following the congress.
After that period, the recordings can be accessed via the e-LIVES library on our website.
Please note that the platform, Video On Demand, and Exhibition can be accessed at any time. Still, our support and live sessions will only be available at the times indicated below:
| Sunday 06 Dec | Monday 07 Dec | Tuesday 08 Dec | Wednesday 09 Dec | |
| Delegate Support | 09:00-19 00 | 09:00-19 00 | 09:00-19 00 | 09:00-19 00 |
| Live Sessions | 14:30-17:00 | 08:45-18:30 | 08:45-18:30 | 08:45-16:20 |
The Help Desk can be contacted from 9.00 am to 7.00 pm (CET) from 06 to 09 December.
To attend the digital congress, you require a valid registration, good internet connection, your computer/laptop and a headset/headphones.
Access is limited to: 1 email / 1 access / 1 device.
You can only connect on one device.
To get the best experience at this digital event, we strongly encourage you to connect using a laptop/PC.
The webcam is not mandatory to attend the event. It will only be necessary for the Meet the Expert sessions.
Pre-registrations for these sessions have sold out and are therefore closed. Registered delegates will receive a special link 24 hours before the session.
Of course, all delegates are very welcome to watch these sessions online, but please note that there is no interactive access for non-pre-registered delegates.
It’s not necessary to be pre-registered to attend the Industry Symposia.
All symposia are accessible to all delegates from the congress platform - just go to your chosen symposium session at the scheduled time.
Yes, those who register for the congress and watch sessions can request a certificate of attendance.
Yes, LIVES Digital is awarded a maximum of 18 CME credits by the European Accreditation Council for Continuing Medical Education (EACCME®). CME credits can ONLY be claimed for participation during the 4-DAY LIVE congress (06-09 December), not for sessions watched after these dates. You are then invited to connect each daily live programme.
To claim your CME credits you need first to complete a short questionnaire about your LIVES Digital experience, which you will receive by email. The CME certificate will then be available to download and/or print.
At the moment, the preliminary programme is available on our website on the e-Planner. The full programme can be viewed on the event platform soon.
The official hour of the entire LIVES Digital 2020 is CET (Central European Time). You can use this website to convert https://24timezones.com/difference/ CET into your local time.
Voting, interactive questions, answer tools, and chat will be available in all live sessions. You will be able to ask a question or make a comment with the speakers during the live sessions.
Yes, if you are a registered delegate you will be able to access all of our sessions and watch them again during 6 months indefinitely and as often as you like.
Industry sponsored sessions and e-booths will be accessible on our platform during 6 months as for the scientific programme.
You will have access to all scientific sessions and on-demand recordings. You will also receive access to the digital exhibition, be able to claim CME credits, review the e-posters, and connect with peers, just as in a physical congress.
LIVES will be an online, digital meeting. Instead of us meeting at a physical location this year for our annual congress, which had been previously planned for Madrid, we will now hold the congress completely virtually and online. More information on how to access the digital congress will come later this autumn.
Please contact your travel agency or flight carrier for questions regarding refunds on travel-related expenses.
Questions related to hotels booked through the conference secretariat need to be directed to hotel@esicm-congress.org
Please contact the Registration Department at registration@esicm-congress.org
CME Accreditation
 CME Accreditation
CME Accreditation
Accredited Continuing Medical Education (CME) is an essential component of continuing physician professional development. Accreditation is of utmost importance - both as proof of the top quality of the congress's scientific content and as an opportunity for delegates to collect their CME credit points.
LIVES Digital programme has been granted 18 European CME credits (ECMEC®s) by the European Accreditation Council for Continuing Medical Education (EACCME®). CME credits can ONLY be claimed for participation during the 4-DAY LIVE congress (06-09 December), not for sessions watched after these dates.
How does it work?
-
- Delegates can exchange their EACCME credits for National CME credits in their home country;
- Physicians may have their EACCME credits converted to AMA PRA Category 1 Credit by applying to the American Medical Association at www.ama-assn.org/go/cme.
Do you have any questions? See our FAQ below.
Yes, those who register for the congress and watch sessions can request a certificate of attendance.
Yes, LIVES Digital is awarded a maximum of 18 CME credits by the European Accreditation Council for Continuing Medical Education (EACCME®). CME credits can ONLY be claimed for participation during the 4-DAY LIVE congress (06-09 December), not for sessions watched after these dates. You are then invited to connect each daily live programme.
To claim your CME credits you need first to complete a short questionnaire about your LIVES Digital experience, which you will receive by email. The CME certificate will then be available to download and/or print.
PROGRAMME
Scientific Programme & Faculty List
 Scientific Programme & Faculty List
Scientific Programme & Faculty List
ESICM has made the decision to make the LIVES 2020 Annual Meeting an entirely virtual event, and we are currently in the processes of transforming the programme to a virtual format.
The programme will be presented in a wide variety of formats – symposia, workshops, case presentations and case discussions. Alongside the dynamic debates and interactive demonstrations, we will provide a wide range of resources on the LIVES Digital 2020 Media Library that can be accessed and viewed on-demand.
All the sessions featured in the video on-demand programme will be available to participants on our digital platform from Sunday 6 December at 14:30 CET. For these presentations, there is neither a set schedule nor a Q&A. This will give all delegates, wherever they may be in the world, the flexibility to watch all the lectures at a time that suits them.
The ESICM LIVES Congress is above all an opportunity for interaction and networking, and LIVES Digital 2020 will be no exception. We will have 7 broadcasting channels at our disposal, allowing a wide-ranging programme of interactive debates, demonstration events, and dynamic presentations/discussions to be sent out live to all the corners of the globe. Check the live channels programme here.
Sessions marked * require Pre-Registrations only available to those who are registered for the main congress.
An application will be made to the UEMS EACCME® for CME accreditation of this event.
Links and all necessary information on how to access LIVES online will be emailed to you on Saturday 5 December.
You will be able to review the sessions and visit the virtual exhibition via the link sent to you (i.e., from the virtual platform) throughout the 6 months following the congress.
After that period, the recordings can be accessed via the e-LIVES library on our website.
Please note that the platform, Video On Demand, and Exhibition can be accessed at any time. Still, our support and live sessions will only be available at the times indicated below:
| Sunday 06 Dec | Monday 07 Dec | Tuesday 08 Dec | Wednesday 09 Dec | |
| Delegate Support | 09:00-19 00 | 09:00-19 00 | 09:00-19 00 | 09:00-19 00 |
| Live Sessions | 14:30-17:00 | 08:45-18:30 | 08:45-18:30 | 08:45-16:20 |
To attend the digital congress, you require a valid registration, a good internet connection, your computer/laptop and a headset/headphones.
No, you can only connect on one device.
At the moment, the preliminary programme is available on our website on the e-Planner. The full programme can be viewed on the event platform soon.
All times given on the LIVES Digital 2020 programme are CET (Central European Time).
You can use this website to convert https://24timezones.com/difference/ CET into your local time.
Voting, interactive questions, answer tools, and chat will be available in all live sessions. You will be able to ask a question or make a comment with the speakers during the live sessions.
Pre-registrations for these sessions have sold out and are therefore closed. Registered delegates will receive a special link 24 hours before the session.
Of course, all delegates are very welcome to watch these sessions online, but please note that there is no interactive access for non-pre-registered delegates.
It’s not necessary to be pre-registered to attend the Industry Symposia.
All symposia are accessible to all delegates from the congress platform - just go to your chosen symposium session at the scheduled time.
Yes, if you are a registered delegate you will be able to access all of our sessions and watch them again during 6 months indefinitely and as often as you like.
Special Sessions
 Special Sessions
Special Sessions
LIVES Digital 2020 will be energized by sessions specially devised to provide participants with a platform for interaction with peers and dedicated experts from the different fields of Intensive Care Medicine.
These informal sessions are meant to encourage participants’ input, peer exchange and the sharing of experience of all the most important issues that impact our profession.
Attendance is limited and requires pre-registration (free of any extra charge). Please note that only those registered for the main congress are eligible for pre-registration.
Meet the Expert Sessions on Channel Berlin
Do you have a burning question for our profession’s leading experts and best-known speakers? Join us for lively interactive debate during this 45-min expert discussion.
Education Case-Based Fundamentals on Channel Paris
Fundamental concepts of intensive care explained by top experts on real cases.
N&AHP Case-Based Fundamentals on Channel Vienna
Learning the fundamentals from simulation of the real-life decision-making made by healthcare professionals in daily ICU practice.
Workshop: Scientific writing - A beginner's guide on Channel Vienna
Introduction to scientific writing: a beginner's workshop.
Journal Club on Channel Milan
In-depth group discussion of a selected scientific paper with internationally renowned experts in the field.
Case-simulation: managing an on call from home on Channel Milan
How would it be if you are on-call at home and your resident calls you about a patient? Will you able to help him and the deteriorating patient?
Do it yourself: Data Science for Intensive Care Medicine on Channel Barcelona
Learn more about how medical data, machine learning and predictive modelling has the potential to provide new insights and improve patient care.
Speakers' Spotlight
 Speakers' Spotlight
Speakers' Spotlight
The LIVES Digital 2020 programme will include 397 live presentations and 365 on demand in a wide variety of formats – symposia, workshops, case presentations and case discussions.
To help you find your way around our extensive programme, we have highlighted some hot topic sessions and speakers.
You can still access the full programme here and the faculty list here.
Sunday 6 December
Channel Madrid
14.30 - 15.30 hrs
The outgoing ESICM President, Jozef Kesecioglu, will officially open the LIVES Digital 2020 congress with a Welcome Address and an update on the Society’s achievements, activities, and future initiatives, ending with the presentation of the Society Medal to one of our long-serving members and the first nurse (and first woman) to receive this award, and deservedly so.
President-Elect, Maurizio Cecconi, will then take to the stage to award Honorary Membership to three individuals who have all made outstanding contributions to the Society and/or the specialty of Intensive Care Medicine.
Chair of the Division of Scientific Affairs, Armand Girbes, will describe what makes this year’s congress the most interactive of all our congresses to date.
 |
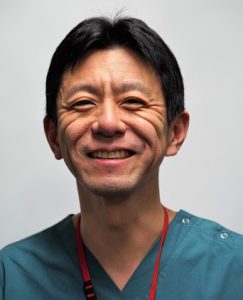
Professor Jozef Kesecioglu (President of the ESICM) is Professor of Intensive Care Medicine at the Department of Intensive Care Medicine at the University Medical Center Utrecht, in the Netherlands.
He completed his medical education and training in anaesthesia and intensive care at the Medical School of the University of Istanbul, Turkey, where he was later appointed as Head of Intensive Care. After moving to the Netherlands in 1989, he worked in Erasmus MC and Sophia Children’s Hospital Rotterdam as an anaesthetist and paediatric intensivist respectively. He moved to AMC in Amsterdam, where he was the Deputy Director, before taking up his current position in 2002. He was responsible for the reorganisation of the four intensive care units at the University Medical Center Utrecht and creating one department, before designing and moving to the new, award winning, state-of-the-art ICU. He has authored more than 150 published or in-press peer-reviewed papers. Before serving the Society as President of ESICM, Prof. Kesecioglu was Chair of the Division of Scientific Affairs and Chair of the Ethics Section. |
 |
Professor Maurizio Cecconi MD FRCA FFICM MD(Res) (President-Elect of ESICM) is Head of the Anaesthesia and Intensive Care Department at the Humanitas Research Hospital, Milan, Italy, and Professor of Anaesthesia and Intensive Care at the Humanitas University, Milan.
Previously, he worked for 14 years as an NHS Consultant at St George’s Hospital, London, United Kingdom. His research focus is on Improving outcomes in Perioperative Care, as well as Data Science and Physiology of Shock, Acute Respiratory Failure, and Sepsis. Prof. Cecconi is part of the Executive Committee of the Surviving Sepsis Campaign and the COVID-19 SSC Guidelines and has worked with WHO on the recent COVID-19 Clinical Guidelines. Since September 2020, he has been overseeing the development of the C19_SPACE training programme funded by the EU. This programme is developed for health care professionals not usually working in ICUs to master the necessary skills to help European hospitals during the second surge of COVID-19 and potential future pandemics. At the beginning of the Pandemic in Europe, he was among the first physicians to warn the rest of the World about the challenges of COVID-19. For his service to the medical and scientific community, he has recently been awarded the knighthood of the order of merit of the Italian Republic. |
 |
Professor Armand Girbes (ESICM Chair of the Division of Scientific Affairs (DSA)) is Professor of Intensive Care Medicine, Clinical Pharmacologist and Chair of the Department of Intensive Care Medicine at VUmc, Amsterdam, in the Netherlands.
From 2003-2009, he was Chairman of the Joint Intensive Care Committee (GIC), where he introduced the European Diploma for Intensive Care (EDIC) - which he helped co-develop within the ESICM (European Society of Intensive Care Medicine) - in the Netherlands. He also developed the system of regular audits in intensive care units in the Netherlands and chaired this body of national audits on quality in intensive care (NKIC) from 2004-2013.He has held various positions within ESICM, including General Secretary, Chair of the Trauma & Emergency Medicine (TEM) Section, EDIC committee, Deputy Chair of the CoBaTrICE (Competence Based Training in Intensive Care in Europe) Committee, and member of the European Board of Intensive Care Medicine. He has authored over 300 scientific publications and as an intensive care trainer at VUmc, has been responsible for the training of more than 120 intensivists. His scientific interests include the methodology of scientific research, vasoactive substances, renal function in heart failure, nutrition, vitamin C and therapeutic hypothermia, in addition to end-of-life care for the patient and their loved ones. |
15.10-15.30 hrs
 |
This year’s Opening Session will also feature a keynote presentation by Lera Boroditsky, Associate Professor of Cognitive Science at UC San Diego and Editor-in-Chief of Frontiers in Cultural Psychology.
|
Discover more about this year’s recipient…
 |
Carole Boulanger is a Consultant Nurse and Advanced Critical Care Practitioner (ACCP) at the Royal Devon & Exeter Foundation NHS Trust (United Kingdom). She is the current elected Chair of the National Association of Advanced Critical Care Practitioners (NaACCP) and a Board representative of the Faculty of Intensive Care Medicine (FICM), in the United Kingdom.
Carole has been involved in the development of the role of advanced clinical care practitioner since its pilot, ten years ago. Alongside practising as an ACCP in her ICU, Carole has been involved in developing the role nationally via the National Framework for Advanced Critical Care Practitioners. She is Honorary Research Fellow to the University of Plymouth and is the immediate Past Chair of the ESICM Nursing & AHP Committee, responsible for developing nursing and AHP activities for the Society. This role not only includes educational provision, but also ensures that nursing and AHP contributions continue to expand as part of the fabric of the Society. |
15:30-15:50 hrs
 |
Professor Mervyn Mer currently presides as a principal specialist at the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa. He also serves as Clinical Head of the Adult Multidisciplinary Intensive Care Unit at CMJAH.
Professor Mer is involved in various aspects of clinical research and postgraduate and undergraduate teaching and serves as an examiner for the Colleges of Medicine of South Africa in several disciplines. He is a past President of the Critical Care Society of Southern Africa (CCSSA) and is the current Chair of the ESICM Global Intensive Care Working Group. He is an invited member of the Society of Critical Care Medicine (SCCM) and ESICM venture that is currently addressing sepsis in developing countries, and in 2018, was invited to become a panel member of the international Surviving Sepsis Campaign guidelines. He also serves as a Council member of the recently formed African Sepsis Alliance. Mervyn has led the theoretical and practical sepsis prevention and management training courses to improve knowledge of sepsis and global infections in resource-limited countries on behalf of the Society’s Fund, ALIVE. |
 |
Dr Heatherlee Bailey, MD FAAEM FCCM, is Assistant Professor of Emergency Medicine at Durham VA Medical Center, North Carolina (USA) and a Past President of the Society of Critical Care Medicine (SCCM) - the first to be trained in emergency medicine.
Dr Bailey is an Emergency Medicine Intensivist and currently practices at the Durham University Medical Center Department of Pathology. She graduated from Rutgers New Jersey Medical School and went on to do a residency at the Medical College of Pennsylvania (known as Drexel University College of Medicine), where she served as Chief Resident. After residency, Dr Bailey created and completed a faculty fellowship of critical care at the Medical College of Pennsylvania. After her fellowship, Heatherlee stayed on at the College where she served in a variety of roles, including Assistant Programme Director, Director of Critical Care Education, and Student Clerkship Director. After this, she transitioned to Duke University, where she served as Director of Critical Care Education before taking her current position at the VA Medical Center in Durham, North Carolina. |
 |
Dr Kent Doi, MD PhD, is Assistant Professor of Medicine in the division of Emergency and Critical Care Medicine at The University of Tokyo, Japan. He received his MD and PhD and residency training at the University of Tokyo Hospital followed by research nephrology training at NIH/NIDDK (2005-2007).
He is a clinical and basic research investigator at the University of Tokyo. His research interests include acute kidney injury and sepsis. His current research involves AKI biomarker development and clarification of pathophysiology of sepsis-induced AKI. Dr Doi is Fellow of the American Society of Nephrology (FASN) and the Japanese Society of Internal Medicine (FJSIM), Councillor and Board Certified Nephrologist of the Japanese Society of Nephrology, Board Certified Senior Member of the Japanese Society of Dialysis Therapy, and Councillor of the Japanese Society for Blood Purification in Critical Care. |
 |
Dr Elisa Estenssoro is Director of the Medical Intensive Care Unit at the Hospital Interzonal General de Agudos "General San Martín" de La Plata, in Buenos Aires, Argentina.
She completed her Fellowship in Intensive Care Medicine in 1988, received her initial Board Certification in Critical Care Medicine in 1988 and Nephrology in 1990. Dr Estenssoro was President of the Argentinian Society of Critical Care (SATI) from 2008 to 2009 and is an active member of the American Thoracic Society. She is additionally a member of the Editorial Board of the American Journal of Respiratory and Critical Care Medicine, and has been Associate Editor of the Annals of the American Thoracic Society (2012-17) and Associate Editor for Latin America of Intensive Care Medicine (2016-2017). Dr Estenssoro's areas of professional expertise and interest include ARDS, Post-ICU syndrome, and sepsis/septic shock. |
15:50-16:05 hrs
 |
Dr John Beigel, MD is Associate Director for Clinical Research, Division of Microbiology and Infectious Diseases, National Institute of Allergy and Infectious Diseases (NIAID).
After his residency at the University of Cincinnati, he completed a fellowship in Critical Care Medicine at the National Institutes of Health and a fellowship in Infectious Disease at the Massachusetts General Hospital. His research interests primarily focus on clinical research and therapeutics in influenza and other emaverging infectious diseases. He has led a portfolio of several multi-center international, FDA regulated (IND) treatment studies for influenza (including plasma therapy and combination antivirals), and most recently has led NIAID’s Adaptive COVID-19 Treatment Trial (ACTT) for advancing therapeutics for COVID-19. |
16:05-16:20 hrs
 |
Dr Kenneth Baillie is a Consultant and Snr. Clinical Research Fellow at Roslin Institute, University of Edinburgh, UK, where he has established a research program in translational applications of genomics in critical care medicine.
He graduated from the University of Edinburgh with a BSc(Hons) in Physiology in 1999 and MBChB in 2002. He completed basic training in medicine in Glasgow and anesthesia in Edinburgh. During this time, he led a series of high altitude research projects in Bolivia and founded a high-altitude research charity, Apex. He was appointed as a clinical lecturer on the ECAT (Edinburgh Clinical Academic Track) at the University of Edinburgh in 2008, and completed a Wellcome Trust-funded PhD in statistical genetics in 2012. He was awarded a Wellcome-Beit Prize Intermediate Clinical Fellowship in 2013. He led a global consensus on harmonisation of research studies in outbreaks for the International Severe Acute Respiratory Infection Consortium (ISARIC), and worked with WHO on H1N1 influenza, MERS, and Ebola. After completing clinical training in 2014, he worked as a visiting scientist at the Broad Institute of Harvard and MIT before returning to the Roslin Institute, University of Edinburgh. He also works as a consultant in the intensive care unit at the Royal Infirmary, Edinburgh. |
16.20 - 16.40 hrs
 |
Dr Enrique Terol MD, is Senior Policy Officer at DG SANTE, in the European Commission and is in charge of the implementation of the European Reference Networks (ERN) under the framework of the Directive of Cross-border Health care since 2011.
He is MD, specialized in Family and Community Medicine, MSc and PhD in Public Health. His professional experience includes the clinical practice, managerial positions of Primary and Specialised Healthcare in private and public institutions and healthcare planning. He was Deputy General Director of Quality and Health Planning of the Ministry of Health of Spain between 2004 and 2008. He worked as Health Attaché in the Spanish Permanent Representation to the EU and coordinator of the area of Health in the Spanish Presidency of the EU between 2008 and 2011. From 2011 to now, he was working as Seconded National Expert and as Policy officer in DG SANTE developing the legal and organisational bases for the set-up of the ERNs. |
 |
Professor Flávia Ribeiro Machado is Professor of Intensive Care at the Federal University of São Paulo, Brazil, where she is Head of the Intensive Care Section of the Anaesthesiology, Pain and Intensive Care Department.
Prof. Machado has become a leading expert in sepsis. She is one of the founders and now CEO of the Latin America Sepsis Institute (LASI), having been its President. She is also part of the Executive Board of the Global Sepsis Alliance and the Executive Committee for the World Sepsis Day. She has served on the board of the Surviving Sepsis Campaign International Guidelines and the International Sepsis Forum (ISF) Council since 2014. With 230 research works and 19155 citations, she has recently been involved in the Executive and Steering Committees of the CoDEX randomised clinical trial to determine whether intravenous dexamethasone increases the number of ventilator-free days among patients with COVID-19-associated ARDS. Flávia will be speaking more on the significance of the trial’s results and answering questions in a Meet the Expert session on Monday 7 December (16.00-16.45 hrs). |
 |
Dr Janet Victoria Diaz is the Unit Head for Clinical Management in the World Health Organisation (WHO) Preparedness Department, responsible for Health Care Readiness and Health Emergency Programming.
As Lead for the Management of Outbreak Response for emerging and re-emerging infectious diseases, Dr Diaz is responsible for the Unit that develops and coordinates clinical operational strategies at a global level. This includes strategies for healthcare workers’ preparedness and supply chain readiness Janet is an accomplished specialist in intensive care medicine with expertise in clinical medicine and global health. She previously served in a clinical capacity at the California Pacific Medical Center, and as MD of the MICU at San Francisco General Hospital, and was Assistant Clinical Professor at the University of California San Francisco. She has published extensively on critical care and pulmonary medicine. |
 |
Professor Sheila Myatra is a consultant intensive care specialist in the Department of Anaesthesiology, Critical Care and Pain at the Tata Memorial Hospital, Mumbai, India, Asia’s largest cancer hospital, where she attends to a 23-bed mixed medical-surgical ICU.
Prof. Myatra is an active member of the ESICM Haemodynamic Section, an appointed member of the ESICM Diversity Task Force and a guest editor of the Society’s official journal, Intensive Care Medicine, since 2019. Another important contribution to the Society is her role of Mentor in the ESICM NEXT Mentoring Programme. Sheila is the lead author of the first published ICU intubation guideline - “Guidelines for Tracheal Intubation in the ICU”, the lead author of the guideline on “Unanticipated Difficult Tracheal Intubation in Adults” by AIDAA, and was the coordinator for the development of the first national difficult airway guidelines (IJA Dec.2016). Sheila has developed a test in hemodynamic monitoring called the “tidal volume challenge” (CCM Mar. 2017) and was one of the 13 international experts to work on the Project for Universal Management of the Airways (PUMA), to develop a universal airway management guideline in 2019. |
Monday 7 December
Channel Milan - 12.00 - 12.20 hrs CET
 |
Professor Margaret S. Herridge is Professor of Medicine, Critical Care and Pulmonary Medicine at the University of Toronto Health Network; Senior Scientist at the Toronto General Hospital Research Institute and Director of Research for the Interdepartmental Division of Critical Care Medicine, University of Toronto.
Margaret is currently Director of the RECOVER Clinical and Research Program for patient-and family-centred follow-up care after critical illness, conducted in collaboration with the Canadian Critical Care Trials group (CCCTG). Her research focuses on understanding the long-term impact of critical illness on patients and their caregivers. She has been awarded the Critical Care Lifetime Achievement Award by the American Thoracic Society in recognition of her research contributions, teaching excellence and service to the Society’s Assembly on Critical Care. She was awarded Honorary Member of the European Society of Intensive Care Medicine in 2019. She has authored or co-authored over 150 manuscripts and book chapters on topics related to outcomes after critical illness in patients and family caregivers and is the co-editor of the textbook of post-ICU medicine with co-editors Doctors Stevens and Hart. She has published two editorials and three manuscripts in the New England Journal of Medicine on outcomes after ARDS and family caregivers after prolonged mechanical ventilation and is a frequent international speaker on outcomes after critical illness. |
Channel Paris, 15:40-16:00 CET
 |
Dr Anders Tegnell is a Swedish physician specialised in infectious disease and the current State Epidemiologist of Sweden.
He studied medicine at Lund University in 1985, later specialising in infectious disease at Linköping University Hospital. In that capacity, in 1990, he treated the first patient in Sweden with a viral hemorrhagic fever, believed to be a case to be either the Ebola or the Marburg virus disease. From 1990 to 1993, he worked for the WHO in Laos to create vaccination programs. From 2002 to 2003, he also worked as a national expert for the European Commission to prepare at the EU level for public health threats such as anthrax, smallpox, and other infectious diseases. Tegnell obtained a research-based senior Medical Doctorate from Linköping University in 2003 and an MSc in Epidemiology from the London School of Hygiene and Tropical Medicine in 2004. After holding several positions in various government agencies, since 2013, he has been serving as Sweden's State Epidemiologist. In this position, he played a key role in the Swedish response to the 2009 swine flu pandemic and the COVID-19 pandemic. Sweden's pandemic strategy has been described as trusting the public to act responsibly: instead of wide-ranging bans and restrictions, authorities have advised people to maintain good hand hygiene, work from home if possible and practice social distancing, while those over 70 have been urged to self-isolate as a precaution. |
Tuesday 8 December
Channel Milan, 9:00-9:45 hrs
 |
Professor Elie Azoulay is Full Professor of Critical Care Medicine and Specialty Pulmonary Medicine at the Paris Diderot University and Vice Chair and Critical Care Director of the Medical ICU of the Saint-Louis Teaching Hospital, Paris, France. In addition, he is Director of the Research Group on the Management of Acute Respiratory Failure and Outcomes in Critically Ill Immunocompromised Patients, the founder and Director of the French FAMIREA Study Group, with 100 centres opened throughout France aimed at improving effectiveness of communication with family members of ICU patients. His research interests include care of the immunocompromised critically ill, pneumonia, as well as ethical aspects of care, including patient and family needs in critical care. His most recent COVID-19 research has covered increased mortality in patients with severe SARS-CoV-2 infection; international variation in the management of severe COVID-19 patients; symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak and a 5-point strategy for improved connection with relatives of critically ill patients with COVID-19. Elie is the current President-Elect of the European Society of Intensive Care Medicine, the former Editor-in-Chief of the Society’s journal, Intensive Care Medicine, and a Past Chair of the ESICM Ethics Section. Throughout the congress, he will join several Round Tables and Interactive Sessions, such as How to handle the COVID-19 crisis: in the ICU and at national level (Monday, Channel Copenhagen, 13:45-14:30 hrs). |
Channel Vienna, 9:45-10:00 hrs
 |
Dr Joanne McPeake is a Nurse Consultant in Clinical Research and Innovation in NHS Greater Glasgow and Clyde, a THIS Institute post-doctoral research fellow (University of Cambridge) and an Honorary Senior Clinical Lecturer at the University of Glasgow (Scotland).
Joanne is actively engaged in working with patients, carers and the lay public in the design, execution and dissemination of research activities. She has set up various patient forums and has published and held research grants with patients and caregivers. Her work has informed Scottish Government policy, including the CMO (Scotland) Realising Realistic Medicine annual report and the Scottish Government’s Health Literacy Action Plan. Joanne has also recently led the development of an international white paper examining the use of peer support as a mechanism to support recovery in critically ill patients. Her principle research interest is related to long term outcomes following critical illness. Specifically, she is focused on how the social determinants of health influence recovery in this group. She also leads an international collaboration aimed at improving long term outcomes for patients and caregivers following critical illness (@CAIROrg). At present, Joanne is PI on a number of national and international studies and collaborates with colleagues from Australia, the USA and Canada. Joanne was awarded the Society of Critical Care Medicine (SCCM) Presidential Citation Award (2018 and 2019) for services to the critical care community. |
Channel Copenhagen, 10:00-10:45 hrs
 |
Dr Lennie Derde is a consultant in ICU and Infectious Diseases in the Intensive Care Centre, University Medical Center Utrecht, in the Netherlands. She is the European co-lead of REMAP-CAP - a trial designed to adapt to an acute pandemic need, which now includes COVID-19 patients.
Dr Derde is the Chair of the Dutch Intensivists Task Force for Infectious Threats and co-author of the ESICM/SCCM/SSC guidelines on COVID-19. She is a member of the ESICM/ESCMID/ERS Severe CAP Guideline Committee and also the Dutch multi-disciplinary committees developing national sepsis guidelines and influenza guidelines. During the congress, she will also moderate the Case-Base Fundamental sessions on Septic shock (Monday, Channel Paris, 9:05-11:45 hrs) and interview Prof. Angus on Publishing in times of pandemics (Wednesday, Channel Copenhagen, 11:00-11:45 hrs). |
Channel Vienna, 14:00-15:00 hrs
 |
Katerina Iliopoulou a post-doctorate fellow at King’s College London and an experienced ex-critical care nurse, passionate about leading change in practice.
She was awarded a doctorate degree in health care from King’s College, London. Her research interests include non-adherence to CLABSIs preventive practices, quality improvement interventions towards infection control and prevention, behaviour change and Critical Care Telemedicine. She strongly supports multidisciplinary collaborations and teamwork in the critical care setting and is an elected member of the European Society of Intensive Care Medicine N&AHP Committee and an active member of the Society’s Journal Review Club. |
Wednesday 9 December
Hot Topics Session, Channel Madrid
14:15-14:30 hrs
"Delirium is common in critically ill patients and associated with impaired short- and long-term outcomes. Non-pharmacologic interventions are recommended in current delirium guidelines, but their effects have not been unequivocally established. Therefore, a multicenter stepped wedge cluster randomized controlled trial was conducted in 1749 critically ill patients to determine the effects of a multicomponent nursing intervention program on delirium in the ICU."
 |
Paul Rood is a former ICU nurse and currently senior researcher within the lectorate ‘Acute and Intensive Care’ and lecturer at the Hogeschool of Arnhem and Nijmegen (HAN) University of Applied Sciences, in the Netherlands. He is a PhD student at the Radboud University Medical Center at Nijmegen (The Netherlands) and is also Vice Chairman of the Dutch Critical Care Nurses Association. |
14:30-14:45 hrs
"The time to diagnosis of invasive Candida infection (ICI) is often too long to initiate timely antifungal therapy in patients with sepsis. Elevated serum (1,3)-β-D-glucan (BDG) concentrations have a high diagnostic sensitivity for detecting ICI. However, the clinical significance of elevated BDG concentrations is unclear in critically ill patients. The goal of this comparative study is to investigate whether measurement of BDG in patients with sepsis and a high risk for ICI can be used to decrease the time to empiric antifungal therapy and thus, increase survival.
Because of the high risk of death, American guidelines recommend empiric antifungal therapy in sepsis patients with a high risk of ICI despite the limited evidence for such a recommendation. In contrast, empiric antifungal therapy is not recommended by European guidelines. BDG may offer a way out of this dilemma since BDG potentially identifies patients in need of early antifungals. However, the evidence for such an approach is inconclusive. This clinical study will generate solid evidence for health-care providers and authors of guidelines for the use of BDG in critically ill patients."
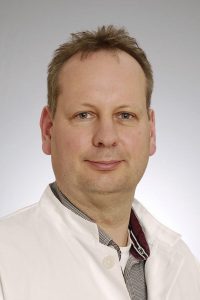 |
Dr Frank Bloos, PhD, is a critical care physician and Principal Investigator at the Department of Anaesthesiology and Intensive Care Medicine at Jena University Hospital (Germany). His research interests include sepsis and anaesthesia. |
15:00-15:15 hrs
"No specific recommendations are available regarding the intensive care management of critically ill acute ischemic stroke (AIS) patients, and questions remain regarding optimal ventilatory, hemodynamic and general ICU therapeutic targets in this population. For this reason, Dr Robba and colleagues performed an international survey, endorsed by ESICM and sent through the NIC Section members, to investigate intensive care unit (ICU) admission criteria and management of AIS patients.
The findings may be helpful to define future studies and create a research agenda regarding the ICU therapeutic targets for AIS patients."
 |
Dr Chiara Robba is a Consultant in General and Neuro Intensive Care and a Researcher at the University of Genova (Italy). She worked for many years in the Neuro Critical Unit of Addenbrooke’s Hospital in Cambridge (United Kingdom).
She received her PhD on Neuromonitoring and the non-invasive assessment of intracranial pressure in 2018. She is the Deputy Chair of the ESICM Neuro Intensive Care (NIC) Section and the author of several publications focused mainly on Neuro Critical Care and Mechanical Ventilation. |
15:15-15:30 hrs
"A consensus of internationally-recognised experts in ICU triage reviewed key challenges of resource driven triage. Recommendations include the following: once available resources are maximally extended, triage is justified utilising a strategy that provides the greatest good for the greatest number of patients.
A triage algorithm based on clinical estimations of the incremental survival benefit (saving the most life-years) provided by ICU care is proposed. “First come, first served” is used to choose between individuals with equal priorities and benefits. The algorithm provides practical guidance, is easy to follow, rapidly implementable and flexible. It has four prioritisation categories: performance score, ASA score, number of organ failures and predicted survival.
Individual units can readily adapt the algorithm to meet local requirements for the evolving pandemic. While the algorithm improves consistency and provides practical and psychological support to those performing triage, the final decision remains a clinical one. Depending on country and operational circumstances, triage decisions may be made by a triage team or individual doctors. Individual institutions may use this guidance to develop prospective protocols that assist the implementation of triage decisions to ensure fairness, enhance consistency and decrease provider moral distress."
Prof. Sprung will provide information about the development of a National policy for the Coronavirus Disease 2019 pandemic and discuss strategies and approaches for policymakers in different countries to develop objective, transparent, equitable and consistent National triage policies.
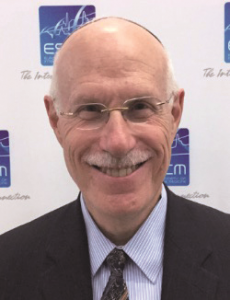 |
Professor Charles Sprung is the Director Emeritus of the General Intensive Care Unit in the Department of Anesthesiology and Critical Care Medicine at Hadassah Hebrew University Medical Center in Jerusalem, Israel, where he has worked for the last 30 years. He was previously the Director of the Section of Critical Care Medicine in the Department of Medicine at the VA Medical Center and the University of Miami for 13 years.
Professor Sprung was the Chairman of the Committee on Ethics Section of the US Society of Critical Care Medicine from 1987 to1994 and of the European Society of Intensive Care Medicine (ESICM) from 1996 to 2001 and 2004 to 2007. He was the Chairman of the Israel Society of Critical Care Medicine from 1990 to 1993 and the Chairman of the Medical and Scientific Subcommittee of the Israel Terminally Ill Law-2005. Professor Sprung has been active in research into sepsis, septic shock and ethical issues for more than 40 years and has published extensively in all of these areas, with more than 300 original publications and 50 books or book chapters. |
15:30-15:45 hrs
 |
Dr Robert Stevens is an associate professor and Director of Precision Medicine for Anesthesiology and Critical Care at The Johns Hopkins University School of Medicine, with appointments in Anesthesiology Critical Care Medicine, Neurology, Neurosurgery and Radiology. He also holds Faculty appointments at the Institute for Data Intensive Engineering and Science (Baltimore) and Johns Hopkins Institute for Computational Medicine.
He is fellowship-trained and board-certified in critical care medicine, neuro critical care, and anaesthesiology. He treats patients with critical illnesses, such as sepsis, ARDS, AKI, traumatic brain injury, trauma, stroke, and immunological disorders of the brain. Dr Stevens’ research uses molecular analysis and imaging to identify specific biologic signatures of injury and illness. This research explores mechanisms of critical illness/injury and recovery, with the goal of discovering and validating patient-specific biological signatures in acute conditions such as traumatic brain injury, cardiac arrest, and sepsis and to validate novel targets for therapy and increase the accuracy of classification and prediction. To achieve this, he has established an interdisciplinary research group composed of biomedical engineers, biostatisticians, data scientists, neuroscientists, systems biologists, and neuro-radiologists. Dr. Stevens is on the Council of the European Society of Intensive Care Medicine and chairs the Committee on Computational Critical Care Medicine at the SCCM. He is an Associate Editor of the journal Thorax, and serves on the Editorial Boards of Critical Care Medicine, Neurocritical Care, and Frontiers in Neurology. Dr Stevens is the principal investigator of the Neuroimaging for Coma Emergence and Recovery (NICER) project, which examines MRI features of the brain connectome to enhance classification and prediction in patients recovering from severe brain injury. |
16:00-16:15 hrs
"Oral chlorhexidine is used widely for mechanically ventilated patients to prevent pneumonia, but recent studies show an association with excess mortality. We examined whether de-adoption of oral chlorhexidine and parallel implementation of a standardised oral care bundle reduces mortality in mechanically ventilated patients using a stepped wedge cluster randomised controlled trial design with integrated process evaluation in 6 ICUs.
3260 patients were enrolled and we found no difference in crude ICU mortality (23.5% (intervention) vs 21.2% (controls), aOR 1.13; CI, 0.82-1.54) or in the time to infection-related ventilator-associated complications (HR 1.06; 95% CI, 0.44 – 2.57). Oral procedural pain (aOR, 0.62; 95% CI, 0.34 – 1.10) was not significantly different, however, oral health dysfunction scores (-0.96; 95% CI, -1.75 to -0.17) significantly improved in the intervention phase.
We concluded that the de-adoption of chlorhexidine and implementation of a standardised oral care bundle may improve oral health and that it is reasonable to impose a moratorium on chlorhexidine use until further evidence becomes available."
Professors Brian Cuthbertson and Craig Dale will be speaking in more detail about their research in a joint presentation at LIVES Digital.
 |
Professor Brian Cuthbertson is an Attending Physician and former Chief of the Department of Critical Care Medicine at Sunnybrook Health Sciences Centre, Canada. He is a Professor in the University Department of Anaesthesiology and Pain Medicine as well as the Interdepartmental Division of Critical Care Medicine at the University of Toronto (Canada).
He is the Vice Chair (Research) in the University Department of Anaesthesiology and Pain Medicine. He is also an Honorary Professor of Critical Care Medicine at the University of Aberdeen (Scotland) and an Honorary Professorial Fellow at the George Institute of Global Health in Sydney, Australia. His research interests include improving outcomes from critical illness and major surgery and he has led a large number of multicentre trials in these areas. He has over 183 peer-reviewed publications, $33million of research grants and an H index of 52. |
 |
Craig Dale RN PhD is an Assistant Professor at the Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, a Scientist at the Tory Trauma Program, Sunnybrook Health Sciences Centre (Toronto), and a Scientist in the University of Toronto Centre for the Study of Pain (UTCSP). His research explores oral hygiene, symptom management, and communication interventions for ventilator-assisted patients and their families. |
Abstract Book & FAQ
 Abstracts
Abstracts
You can access ESICM LIVES Digital 2020 Abstract Book here.
All ESICM Abstract Books from 2014 to 2020 can be found here.
Guidelines & Instructions
Best Oral Presentations (live Q&A session will be run*)
This would take the form of a 3 minute pre-recorded presentation of your research, followed by a 3 minute live discussion between you as speaker and a moderator.
*There will be audience questions via a chat facility with questions selected by the moderator.
Please keep the number of slides to a minumum - we would suggest no more than three. We recommend that you:
- start with your conclusion slide
- support your conclusions with the most relevant data
- end with a take home message
Please click here for the PowerPoint template.
Oral Presentations (no live Q&A session will be run*)
Your 3 minute pre-recorded presentation should take the form of an audio recording accompanied by one single slide. This programme includes a zoom-in facility which allows the viewer to select the different features of the slide and hear the accompanying audio.
*There will be audience questions via a chat facility, and we would ask you to be available to give answers when you receive a question notification.
Please click here for the PowerPoint templates (chose one from the two available).
e-Posters (no live Q&A session will be run*)
Your presentation should take the form of one single PowerPoint slide.
*There will be audience questions via a chat facility, and we would ask you to be available to give answers when you receive a question notification.
Please click here for the PowerPoint template (chose one from the two available).
Review Process
The abstract submission system closed on 30 July 2020. This abstract receipt deadline will remain firm and any abstracts received after the deadline will not be accepted.
The authors have been informed of acceptance/rejection of their abstract by email on 22 September and 05 October.
A platform to record and upload abstracts will be available from 20 October, an individual link has be sent along with the guidelines. This process has been delayed due to the COVID-19 situation.
Still have questions? See our FAQ below.
No, your slide has to be uploaded and will be published on the LIVES Digital platform during the whole congress duration. No live Q&A session will be run. However, there will be audience questions via a chat facility, and we would ask you to be available to give answers when you receive a question notification.
Yes, all accepted abstracts will be published in the Abstract Book which can be accessed via our website just before the congress.
Yes, all participants who submitted an abstract will receive a certificate after the congress.
Abstract notifications have been sent to the presenting authors on 22 September and 05 October. This is later than was planned due to the COVID-19 situation.
No, you will not be able to make changes to your abstract once submitted. However, corrections can be highlighted on your poster if necessary.
No, late-breaking abstracts won’t be accepted.
Yes, the abstract presenter must register for the congress in order to present his work.
Yes, all presenters of accepted abstracts are required to present their poster during the digital event. More details of how to submit your presentation will follow by email in the coming weeks.
What happens if I have planned to present my abstract at another congress before LIVES Digital 2020?
Submitting an abstract also certifies that at the time of submission, the scientific material found within the abstract has not been presented at any other meeting and will not be published in any form other than abstract form prior to LIVES Digital 2020. If you have plans to do so, please contact us at scientific@cyim.com in order that your abstract may be withdraw from our event.
Although you may withdraw your abstract and decide not present it during the LIVES 2020 digital congress please note that this will mean you will not be able to submit it again for LIVES 2021, as the abstract will have already been published in the Abstract Book 2020.
Please email us at scientific@cyim.com
Best Abstracts
 LIVES Digital 2020 Abstracts Awards
LIVES Digital 2020 Abstracts Awards
Three N&AHP Best Abstract Awards
The N&AHP Best Abstract Awards include three free registrations to LIVES 2021 (core congress).
Abstracts selected by the jury will be presented in our session N&AHP research & networking: What's new? during the Digital Congress on Monday 07 December between 14:00-16:15
- Cross-sectional validity of the Chelsea Critical Care Physical Assessment tool (CPAx) in critically ill adults - S. Eggmann (Bern, Switzerland)
- Impact of a nurse-led family support intervention for families of critically ill persons: A mixed methods study - P. Massarotto (Zürich, Switzerland)
- The role of the physiotherapy team in a multidisciplinary management of pronation in critically ill COVID-19 patients - S. Ceruti (Lugano, Switzerland)
One ISF Abstract Award
The ISF Abstract Award includes a free registration to LIVES 2021 (core congress).
Abstract selected by the jury will be presented in our session Best Oral Presentations 1 during the Congress on Monday 07 December at 14:00-15:00
- Involvement of β-adrenergic modulation in lymphocyte balance during experimental septic shock - M. Durand (Nancy, France)
Thirty Best Abstracts
Presenters of the 30 best abstracts will receive an award, including one free registration to LIVES 2021 (core congress).
Abstracts selected by the jury will be presented in our sessions Best Oral Presentations 1-2-3 during the Congress between 07-09 December
- Identification of novel clinical subphenotypes in patients with community acquired pneumonia. A derivation study - Aquino Esperanza Jose, Spain
- Effects of high flow nasal cannula (HFNC) in patients with sepsis and septic shock of extrapulmonary origin - Basile Maria Cristina, Italy
- (1,3)-β-D-glucan-based diagnosis of invasive Candida infection versus culture - based diagnosis in patients with sepsis and with an increased risk of invasive Candida infection (CandiSep) - Bloos Frank, Germany
- Efficacy and Safety of Imipenem/Cilastatin/Relebactam Versus Piperacillin/Tazobactam in Patients With Hospital-Acquired Bacterial Pneumonia/Ventilator-Associated Bacterial Pneumonia by Geographic Region - Chen Luke F, United States of America
- H and L-subphenotype prevalence in ARDS patients with and without SARS-CoV-2 - Chotalia Minesh, United Kingdom
- Impact of oral chlorhexidine de-adoption and implementation of an oral care bundle on mortality for mechanically ventilated adults: A stepped wedge cluster randomized controlled trial - Dale Craig, Canada
- Temporary transvenous diaphragm neurostimulation in mechanically ventilated patients – preliminary results from a randomized controlled trial - Dres Martin, France
- Involvement of β-adrenergic modulation in lymphocyte balance during experimental septic shock - Durand Manon, France
- Cross-sectional validity of the Chelsea Critical Care Physical Assessment tool (CPAx) in critically ill adults - Eggmann Sabrina, Switzerland
- Role of endothelial micro RNA 155 on capillary leakage in systemic inflammation - Etzrodt Valerie, Germany
- The association between the Sequential Organ Failure Assessment scores in particular systems and intensive care unit mortality in patients ≥80 years old – a prospective cohort study - Fronczek Jakub, Poland
- Dysphagia and evolution during COVID-19 pandemic in critically ill patients. A multidisciplinary challenge for healthcare workers - Glotta Andrea, Switzerland
- Where did all the women go? The underrepresentation of women in educational resources during COVID-19 - Hall Tanya, United Kingdom
- Biological subphenotypes of acute respiratory distress syndrome show prognostic enrichment in the general ICU population - Heijnen Nanon, Netherlands
- Vasoactive effects of vanilloids in progressive peritoneal sepsis - Horak Jan, Czech Republic
- PEEP titration with electrical impedance tomography and pressure-volume curve: a randomized trial in ARDS patients - Hsu Hui Ju, Taiwan
- Long-term developmental impact of withholding parenteral nutrition in paediatric-ICU: a 4-year follow-up of the PEPaNIC randomized controlled trial - Jacobs An, Belgium
- Moderately prolonged permissive hypotension results in reversible cerebral metabolic perturbations evaluated by intracerebral microdialysis - Jakobsen Rasmus Peter, Denmark
- Randomized Clinical Trial Comparing Gram Stain-guided Initial Antibiotic Treatment with Guidelines-based Treatment in Patients with Ventilator-associated Pneumonia: GRam stain-guided Antibiotics ChoicE for Ventilator-Associated Pneumonia (GRACE-VAP) Trial - Jumpei Yosimura, Japan
- Effects of prone positioning on venous return in patients with acute respiratory distress syndrome - Lai Christopher, France
- Circulating bioactive adrenomedullin as a marker of sepsis, septic shock and critical illness - Lundberg Oscar H M, Sweden
- Epidemiology and risk factors of ventilator-associated pneumonia in COVID-19 patients: a propensity-score matched analysis - Martinez Martinez Maria, Spain
- The use of high flow nasal cannula oxygen around end of life: indications, complications, outcomes - Metaxa Victoria, United Kingdom
- Relationship between obesity and ventilator-associated pneumonia: a planned ancillary study of the NUTRIREA-2 randomized controlled trial - Nseir Saad, France
- Different renal trajectories and outcomes after Acute Kidney Injury in Intensive Care Unit: a 5-years prospective cohort study- Orieux Arthur, France
- “Is this a good time to talk?” Improving telephone communication between junior doctors and relatives of patients in ICU during the COVID-19 pandemic - Rahim Anika, United Kingdom
- Validation of a novel non-invasive continuous method to monitor end expiratory lung volume based on CO2 kinetics - Sánchez Giralt Juan Antonio, Spain
- Impact of sex and ICU treatment duration on creatinine and potassium excretion in critically ill patients - Van Bakelen-Knip Martine, Netherlands
- Incidence and risk factors of deep vein thrombosis after extracorporeal membrane oxygenation - van Minnen Olivier, Netherlands
- Evidence of Heart Decoupling Between Work, Metabolism and Microcirculation in Endotoxic Shock : [11C] Acetate PET Approach - Visinoni Nicolas, France
REGISTRATION
Registration Information
 Registration Information
Registration Information
If you have registered for the congress, you should have received an email with information on how to access the congress, complete with URL and login details.
Registration for LIVES Digital 2020, our fully digital and interactive annual congress, opens on 1st October.
ESICM is rewarding all its members who register between Thursday 1st October and Thursday 8th October, FREE REGISTRATION for our digital congress. This offer is for a limited period only, so do not delay!
After 8th October, standard fees will apply and ESICM members can still benefit from special reductions on the congress fee, set out below.
NB: The fees are net and that 21% Belgian VAT will be added (if applicable).
| ESICM Members | Early fees 1 Oct to 8 Oct |
Standard fees 9 Oct to 9 Dec |
| Physician | 0 € | 60 € |
| In Training, Nurses & AHPs | 0 € | 40 € |
| Non-Members | Early fees 1 Oct to 5 Nov |
Standard fees 6 Nov to 9 Dec |
| Physician + (up to the end of 2020 + 2021 full membership) |
160 € | 220 € |
| In Training, Nurses & AHPs + (up to the end of 2020 + 2021 full membership) |
120 € | 160 € |
| Physician | 90 € | 140 € |
| In Training, Nurses & AHPs | 40 € | 90 € |
NB: Registrations for more than 10 (ten) participants will be handled separately as a group booking. Please contact the ESICM Registration Department by Email
If you are not yet a member of ESICM, there is no better time to join.
Join now! and benefit from this offer and all the other advantages membership of our global intensive care community brings.
More information about ESICM membership fees, HERE
Registration Dates
FOR MEMBERS
Free registration: until 8 October 2020, 23:59 CET
Standard registration: from 9 October 2020
FOR NON-MEMBERS
Early registration: until 5 November 2020, 23:59 CET
Late registration: from 6 November 2020
Registration Department
K.I.T. Group GmbH
Association & Conference Management
Kurfürstendamm 71
10709 Berlin
Germany
Tel: +49 (0)30 24 603 319
Email
**** Important Alert ****
There are an increasing number of fraudulent websites and individuals that impersonate ESICM and our Annual Congress, but that are in no way associated with ESICM.
We would like to alert all our members and delegates to be aware of companies claiming to be ESICM partners and we strongly advise you to only use our official Congress registration partner, KIT.
Please also pay attention to fraudulent websites. There is only one ESICM LIVES Digital 2020 Website and ESICM’s only official provider of housing and registration is KIT Group GmbH.
ESICM will not accept any responsibility for bookings made via unofficial websites and agencies.
SPONSORSHIP AND EXHIBITION
Opportunities & FAQ
 Sponsoring
Sponsoring
Why support LIVES Digital 2020?
LIVES Digital 2020 will be hosted on the ESICM media library, e-LIVES. This online educational tool provides unbiased, high quality,interactive continuing medical and professional education in the fields of Intensive Care.
We have structured the LIVES Digital 2020 programme to maximise its global reach, taking into account the many different locations and time zones of our participants, whether they are working in Europe, Africa, Asia, the Americas or Oceana. Delegates will be able to attend all the key presentations at a time that suits them!
How and what will the digital programme deliver?
The programme covers the most recent research advances, developments and treatments, in a wide variety of formats –symposia, workshops, case presentations and case discussions.
Our focus is on optimising the interaction between the faculty and audience to enhance the learning process for all our delegates.
We will be actively encouraging the exchange of knowledge between clinical practitioners, researchers, established investigators, physicians, nurses, allied health professionals, doctors in training and medical students, offering multiple interactive sessions and networking opportunities.
What are the expected educational outcomes?
In summary, LIVES Digital 2020 allows delegates to:
- update their knowledge
- discuss real life cases to help them diagnose and treat patients in their daily practice
- receive data and information about the latest research findings in Intensive Care
- take part in state-of-the art symposia to complement and complete their knowledge of Intensive Care
JOIN US!
For the LIVES Digital 2020 exhibition or Sponsorship opportunities, please contact
Sponsorship/Exhibition
For questions regarding sponsorship and the ESICM LIVES 2020 Digital, please contact:
Joel Alexandre
ESICM CEO
Email: Joel.alexandre@esicm.org
Ms Valerie Farrow
ESICM Congress department
Email: valerie.farrow@esicm.org
K.I.T. Group GmbH
Ms Elena Baggetta & Ms Jean Modräger
Tel.: +49 30 24 603 -345
Email: lives2020-industry@kit-group.org
Still have questions? See our FAQ below.
Please contact lives2020-industry@kit-group.org.
The industry registration allows access to the Industry Symposia, live stream for Industry Meet the Experts sessions and the Industry Exhibition Hall.
Please register as AHP at https://www.esicm.org/events/33rd-annual-congress-madrid/registrationlives2020/.
For the booth representatives, we suggest the following times:
- Sunday 6 December: 12:00 – 17:00 CET
- Monday 7 December: 09:00 – 17:00 CET
- Tuesday 8 December: 09:00 – 17:00 CET
- Wednesday 9 December: 09:00 – 12:00 CET
Each exhibitor can independently define when to be available to chat.
The exhibition booths will be online until May 2021 on the congress platform of the ESICM Digital Congress 2020. The chat function will be disabled after the congress.
The webcast of the Industry Sessions will be available until May 2021 on the congress platform of the ESICM Digital Congress 2020.
Further to that, it will be available on ESICM's media library for 3 years.
Sponsors & Exhibitors
The ESICM would like to wholeheartedly thank the following companies who are entitled to be recognised as:
Sponsored Sessions
Industry sessions, organised by leading medical device and pharmaceutical companies, provide delegates with an in-depth view in innovations, developments and progress related to intensive care. Industry Symposia and Meet the Expert Sessions are organised outside the scientific programme to provide delegates with an opportunity to attend. These sponsored programmes do not form part of the official scientific programme of LIVES. By attending those sessions, please be aware that you will be giving permission for your personal details to be shared with the company holding the industry sessions. Sessions marked * require Pre-Registrations (free of any extra charge) only available to those who are registered for the main congress. Industry Sponsored Sessions
Industry Sponsored Sessions
12:30 to 13:30 - Symposia

08:45 to 09:15 - Meet the Experts*
12:30 to 13:30 - Symposia
18:00 to 18:30 - Meet the Experts *


































