High Flow Nasal Cannula in adult patients: a review of practice clinical guideline
New guideline addressing the role of High Flow Nasal Cannula oxygen delivery as an alternative mode of respiratory support in different clinical conditions
HFNC is a non-invasive interface that allows for delivering high flow (30-60 L/min) of heated and humidified gas at predictable FiO2 between 0.2 and 1.0. Given these advantages and its apparent beneficial physiological effects, the use of HFNC has been increasing over the last few years, although the evidence supporting its application remains limited.
This guideline aims to explore the role of HFNC in four clinical scenarios (hypoxic respiratory failure, peri-intubation, post-extubation and post-operative) and compare it to other respiratory-support strategies such as conventional oxygen therapy (COT), CPAP and NIPPV.
The guideline was developed by a panel of experts nominated by ESICM.
The panel developed four questions according to PICO (Patients, Intervention, Comparator, Outcomes) criteria. It used the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach to assess the quality of evidence for each question’s outcome and the strength of recommendations.
The panel made four recommendations, all with moderate certainty of evidence, based on the results of RCTs and meta-analysis:
- Strong recommendation for HFNC compared to COT in hypoxemic acute respiratory failure.
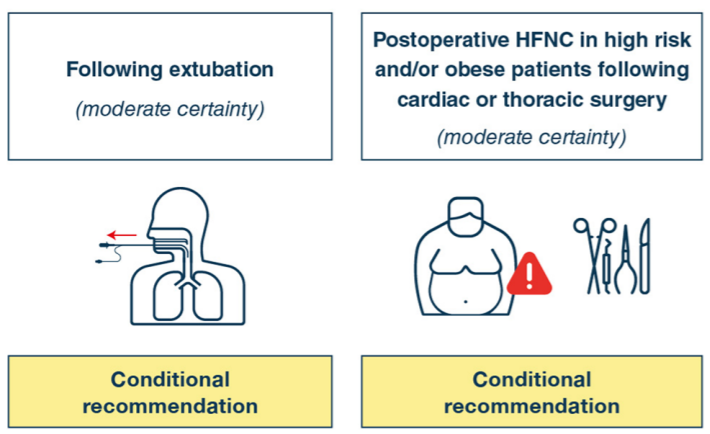
- Conditional recommendation for HFNC compared to COT following extubation in high-risk patients who are intubated for more than 24 hours.
- No recommendation for HFNC in the peri-intubation period.
- Conditional recommendation for post-operative HFNC compared to COT in high-risk and obese patients who underwent cardiothoracic surgery.
The guideline focuses on the comparison between HFNC and COT. HFNC has been demonstrated to be superior to COT in preventing intubation and escalation of respiratory support in hypoxemic patients. HFCN has also been proved to reduce the rate of re-intubation, the incidence of post-extubation respiratory failure and the need for escalation of respiratory support in high-risk patients.
Insufficient evidence is available on the use of HFNC as opposed to NIPPV in these clinical settings to allow the panel to draw conclusions.
STUDY STRENGTHS & LIMITATIONS
Strengths
- Focus on clinical conditions where the use of HFNC is widespread but highly variable in everyday practice.
- Rigorous methodology: comprehensive search and systematic review of the literature, inclusion of recent published evidence, evaluation bias risk of individual RCTs, application of GRADE system.
- Importance given to research priorities to guide future investigations.
Limitations
- Insufficient data to perform subgroup analysis and identify, in each clinical scenario, the patients who would benefit the most from HFNC.
- No recommendations on settings, prediction of failure, timing and methods to wean from HFNC, since there is no evidence available.
- Exclusion of patient representatives from the panel.
TAKE HOME MESSAGE
Indications for HFNC oxygen therapy are expanding as evidence on this new technology is growing. According to the ESICM guideline, HFNC is recommended in patients with acute hypoxemic respiratory failure, it is suggested following extubation and post-operative in high-risk patients and it is not recommended in the peri-intubation period.
This article review was prepared and submitted by Drs. Marta Cicetti and Dr. Temistocle Taccheri, Fondazione Policlinico A. Gemelli IRCCS, Rome (Italy), on behalf of the ESICM Review Journal Club.
REFERENCES
Rochwerg, B., Einav, S., Chaudhuri, D. et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med 46, 2226–2237 (2020).
Rochwerg, B., Granton, D., Wang, D.X. et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive Care Med 45, 563–572 (2019).