Expanding cDCDD – an article review by the NEXT Committee

Expanding controlled donation after the circulatory determination of death: statement from an international collaborative
This Article Review was created by Andrea Ortiz Suñer, Intensive Care Unit, Intensive Care Unit, Hospital Arnau de Vilanova, Valencia (Spain), on behalf of the NEXT Committee
Seeking to implement the World Health Organization (WHO) Guiding Principles on the Human Cell, Tissue and Organ Transplantation throughout the world in all countries with deceased organ donation, both WHO and The Transplant Society (TTS) had worked on this statement to guide protocols who included organ donation in the pathways to death.
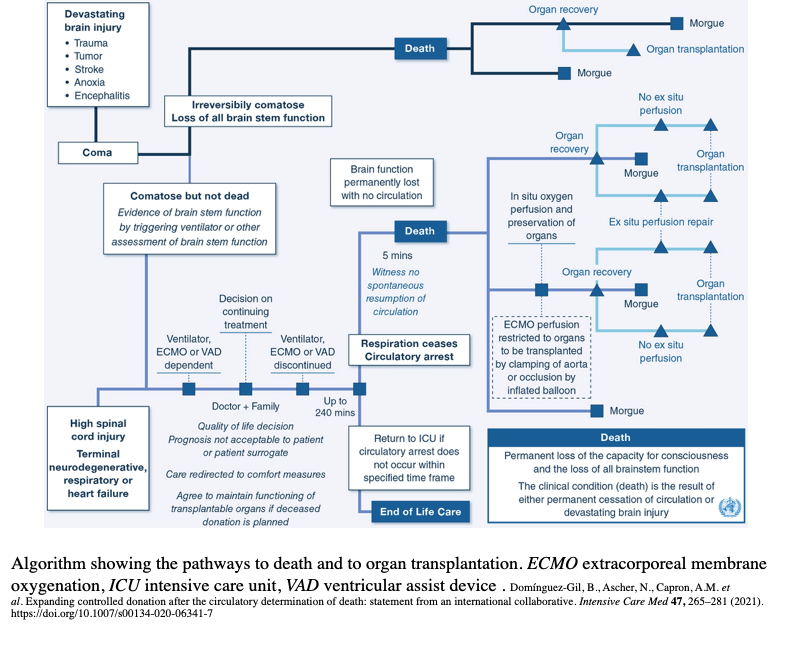
Expanding deceased donation increases the opportunity to help patients in need by donating organs after death when this is consistent with their intended values. Most cases involve donation after neurological determination of death (DNDD), this Statement focuses on donation after circulatory determination of death (DCDD). Controlled DCDD (cDCDD) refers to organ donation from a patient who has died in the hospital following the withdrawal of life-sustaining treatment (WLST). Uncontrolled DCDD refers to donation after a failed effort to resuscitate out-of-hospital or unexpected in-hospital cardiopulmonary arrest.
The Statement is based on three fundamental points. First, the WLST should be prior to and independent of any other consideration. The aim is to consider the possibility of cDCDD as a routine component of end-of-life care. The process of determining a prognosis and the decision to WLST should exclude transplant healthcare professionals. The conditions in which the WLST is undertaken include devastating brain injury, high spinal cord injury, terminal neurodegenerative diseased respiratory or heart failure. The decision to WLST should be delayed up to 72h, time enough to administer appropriate treatment in the ICU which will improve the reliability of establishing the poo prognosis.
Secondly, it remarked that death should be declared after permanent cessation of circulation to the brain. The elapsed observation period of 5 min without circulation to the brain, confirms the absence of brain functions is permanent (nor capacity for cons piousness, breath or all other brainstem functions). Validated tests to verify the circulatory cessation are the absence of arterial pulsation, aortic valve opening, doppler circulation or electrical activity. Nevertheless, using electrocardiogram may prolong unnecessarily warm ischaemia.
And finally, it is highlighted the value of perfusion repair in increasing the success of cDCDD organ transplantation. In situ or ex situ organ preservation and repair could be protocoled for cDCDD. Warm ischaemia is inherent to the cDCDD process, related to progressing hypoxemia and hypotension after WLST, and could damage organs, liver and heart particularly. Being the heart the most sensitive to ischaemia, both cold and warm, several factor should be addressed for a cDCDD program, like the use of heparin, no-touch period between systole to declaration of death and time from systole to cardioplegia.
In situ normothermic regional reperfusion (NRP) using an ECMO (extracorporeal membrane oxygenation) device could be achieved using ante or post-mortem cannulation, but it has ethical challenges. Restoring the brain circulation is the most critical one, it would invalidate the death determination. Techniques used for isolating the brain must be used including balloon occlusion or surgical clamping. NRP seems to reverse the metabolic derangements caused by warm ischaemia and may attenuate ischaemia-reperfusion injury. NRP is also associated with decreased rate of overall biliary complication, ischaemic type biliary lesions and graft loss. Donors ages of cDCDD liver could be expanded safely with NRP. Kidney and lung experience with NRP is scarce for now.
STATEMENT RECOMMENDATIONS
• Pertaining to the process of determining a prognosis that justifies the withdrawal of life-sustaining treatment.
• Health authorities, professionals and professional associations should evaluate the circumstances of patients dying in ICUs. In countries where WLST is an accepted practice in the consideration of treatment futility and end‐of‐life care, the possibility of developing a cDCDD program as a routine component of end‐of‐life care should be explored.
• The cDCDD program must be developed with a comprehensive regulatory framework that emphasizes the independence of organ donation.
• Transplant healthcare professionals must not be involved in reaching the decision to WLST nor in the actions involved in the WLST.
• Pertaining to determining death after the permanent cessation of circulation to the brain.
• In cDCDD, death may be declared after an elapsed observation period of 5 min without circulation which confirms that the absence of circulation is permanent. The permanent absence of circulation to the brain results in the permanent absence of brain functions.
• Transplant professionals caring for potential transplant recipients should not be involved in the determination of death.
• Pertaining to perfusion repair for increasing organ transplantation success in cDCDD.
• The value of perfusion for increasing the success of organ transplantation is established by this Conference Statement to recommend that a protocol of cDCDD utilize either in situ or ex situ perfusion consistent with the practice of each country conducting cDCDD.
TAKE-HOME MESSAGE
When the decision of WLST is considered and accepted, cDCDD should be included in the possibilities when is consistent with the patient’s wishes and values.
Transplant healthcare professionals should not take part nor the decision of WLST or the determination of death.
For organs in situ preservation, ECMO perfusion should be restricted to organs to be transplanted by clamping or occlusion of the aorta.
REFERENCE
Domínguez-Gil B., Ascher N. Capron, A.M. et al. Expanding controlled donation after the circulatory determination of death: statement from an international collaborative. Intensive Care Med 47, 265–281 (2021). https://doi.org/10.1007/s00134-020-06341-7
NEXT is a Steering Committee that speaks on behalf of trainees/young specialists and helps shape the future of the European Society of Intensive Care Medicine (ESICM) and of the discipline. Would you like to join us? Visit https://www.esicm.org/the-esicm/membership/ and follow us on Facebook | Twitter | Instagram.
Disclaimer: This short review was created because the original publication from which it is derived was judged to be relevant in the field of Intensive Care Medicine. The original publication is available for full consultation at the journal’s website. The creator is not related in any way to the original publication.