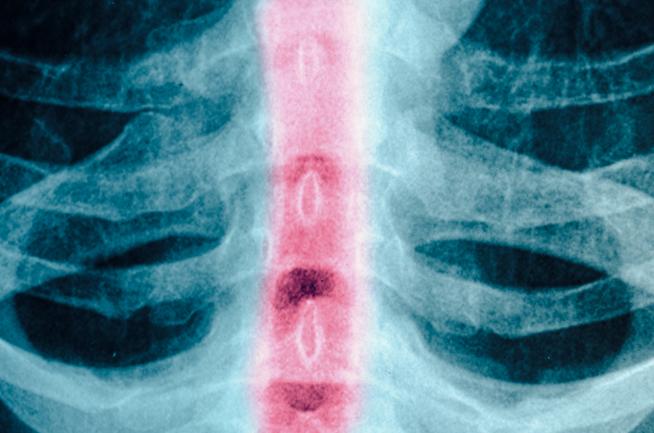
Continuous Monitoring of Spinal Cord Pressure Possible after Spinal Cord Injury
ARTICLE REVIEW
Currently, there is no consensus on blood pressure management or optimal SCPP after tSCi, but recommended mean arterial pressure (MAP) of 85-90 mmHg for 5-7 days after tSCI (1). It may also be difficult to use imaging and clinical examination for guiding tSCI management. Moreover, there is no method in clinical use for measuring ISP after tSCI analogous to measuring intracranial pressure after TBI.
In the recent article “Monitoring of Spinal Cord Perfusion Pressure in Acute Spinal Cord Injury: Initial findings of the Injured Spinal Cord Pressure Evaluation Study” (Critical Care Medicine, March 2014), the authors propose a feasible technique to monitor ISP for up to one week without complications.
Study Design
Board-certified neurosurgeons placed a pressure transducer probe subdurally (at the site of maximal spinal cord swelling according to MRI) following laminectomy or small laminotomy and tunnel it through the skin into the surgical wound. With increasing experience the pressure probe placement in the spinal cord was shown to be simple, requiring about 10 minutes.
18 patients with tSCI (American Spinal Injuries Association [ASIA] grade A-C) were successfully enrolled and compared to 2 different populations of control subjects: 1) patients investigated for normal pressure hydrocephalus that had normal cerebrospinal fluid (CSF) dynamics (spinal cord pressure parameters); 2) patients admitted for elective surgery for cervical or lumbar radiculopathy (Motor Evoked Potentials, MEPs).
The parameters recorded for one week are ISP, MAP (through invasive blood pressure monitoring) and the calculated ones are SCPP (MAP-ISP), spinal pressure reactivity index (sPRx, a measure of spinal cord vascular reactivity) and spinal reserve capacity index (sRAP, a measure of compensatory reserve).
All patients were assessed clinically (limb motor score) and neurophysiologically (MEPs) at different levels of SCPP (changed using noradrenaline or metaraminol).
Findings
The authors found the following: no complications related to ISP monitoring (such as wound infection, meningitis, CSF leak, pseudomeningocele, spinal cord or subdural haematoma or deterioration in ASIA score); a progressive loss of autoregulation for increasing ISP values and low SCPP (below the optimal level calculated through sPRx) and increased ISP at the injury site compared to a lower CSF compartment or extradurally; no significant changes in ISP or SCPP with changes in PaCO2, mannitol 20% bolus iv and incresed sevoflurane whereas vasopressors increased MAP and ISP with a net increase in SCPP; transient low SCPP (<60 mmHg) despite recommended MAP (85-90 mmHg); improved MEPs responses to increased SCPP.
Due to the small number of patients recruited and used for some of the subanalysis in the present study no defined conclusions about the recommended management of blood pressure after tSCI can be defined. However, this study suggests that optimal SCPP may vary between patients and should be individualised.
Take Home Message
The authors demonstrated through this feasibility study that it is possible to continuously monitor subdural spinal cord pressure (ISP) for up to a week without complications after traumatic spinal cord injury (tSCI).
Findings also suggest that the cord is ischaemic after tSCI. Interestingly, some interventions used to lower intracranial pressure after traumatic brain injury (TBI) may be ineffective to lower ISP and improve the spinal cord perfusion pressure (SCPP) in tSCI.
Future applications of ISP monitoring are broad both for clinical and research purposes
Clinical Implications
– Blood pressure management following tSCI
– Optimal SCPP monitoring and management
However this study suggests that further research is required to better understand:
– the pathophysiology of ISP and SCPP following tSCI
– the best clinical correlates to use as outcome measures
– the value of calculated parameters such as sPRx and sRAP
This article review was prepared and submitted by Lara Prisco, Chair of the NEXT Committee, with assistance from Dr. Mario Ganau, Neurosurgeon.
Reference
- Werndle MC, Saadoun S, Phang I, Czosnyka M, Varsos GV, Czosnyka S, Smielewski P, Jamous A, Bell A, Zoumprouli A, Papadopoulos MC. Monitoring of Spinal Cord Perfusion Pressure in Acute Spinal Cord Injury: Initial findings of the Injured Spinal Cord Pressure Evaluation Study. Critical Care Medicine, March 2014, Volume 4 / Number 3