The risk and clinical outcome of candidemia
The risk and clinical outcome of candidemia
EJRC ARTICLE REVIEW
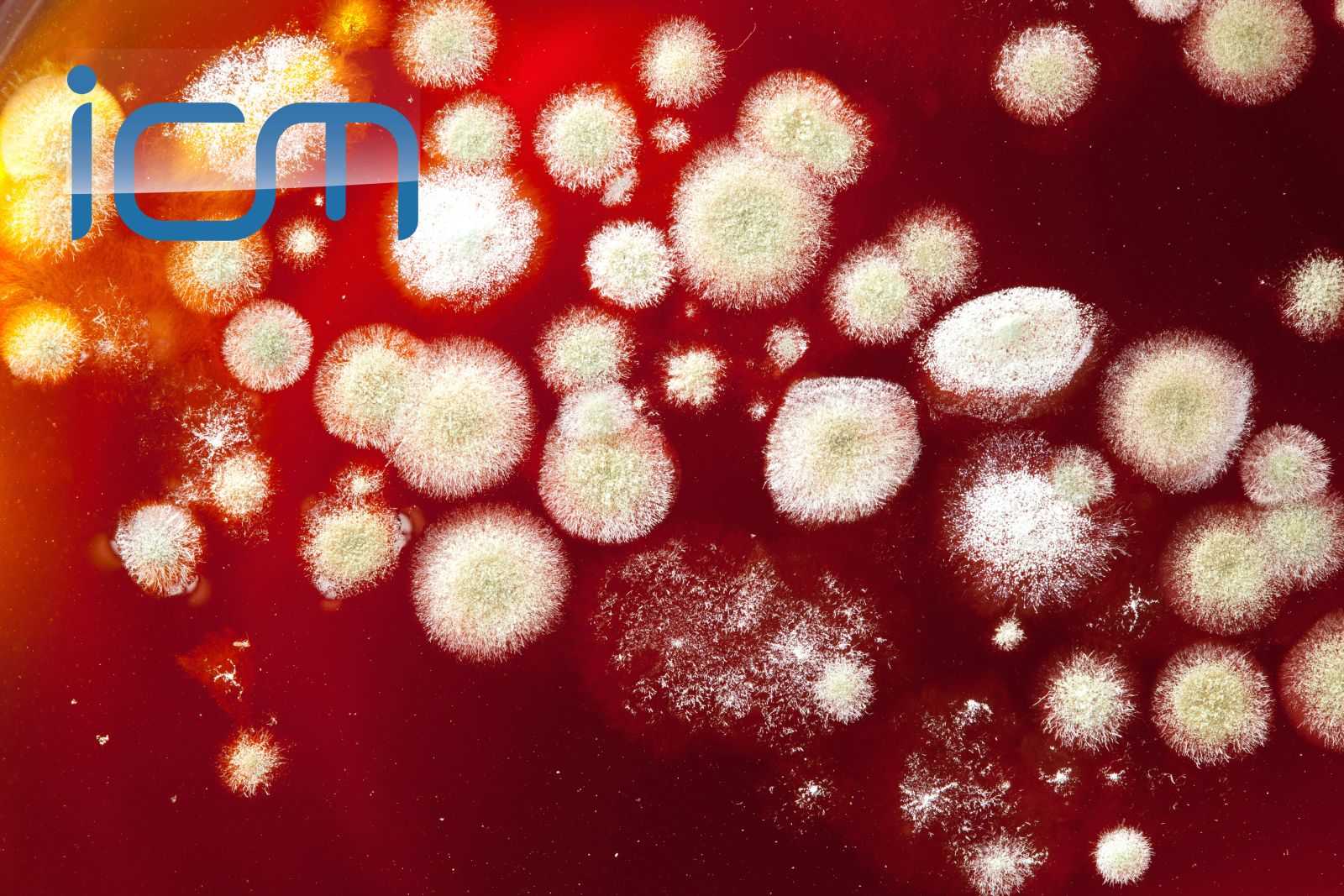
Candidemia incidence has been increasing over the past decade, becoming the fifth most common nosocomial bloodstream infection. Currently, several species of Candida and different risk factors have been recognised. The authors of this prospective multicentric hospital-based surveillance programme investigated candidemia distribution and outcome in a large cohort of critically ill patients according to their underlying disease.
Between October 2002 and December 2014, 3417 patients from 26 university hospitals from the Paris area were studied: almost half of them (47.2%) were hospitalised in ICU. 586 patients (17.1%) had haematological malignancies (mainly lymphoma and acute leukemia), 1164 patients (34.1%) had solid tumors (“oncology” group) and 1667 patients (48.8%) had no malignancies.
Fluconazole and echinocandins were the most frequent first-line antifungal treatments and a trend towards an increased prescription of echinocandins as first-line treatment, compared to fluconazole, was observed during the study period.
Mixed infections represented 3.3% of all episodes, involving mostly C.albicans and C.glabrata. The former was overall the predominant species, but its proportion compared to the others varied with the underlying disease and ICU hospitalisation. In patients hospitalised in ICU with acute leukemia, C.tropicalis was almost as frequent as C.albicans. C.parapsilosis was less frequent in ICU than outside ICU for all patients with malignancies
A multinomial analysis revealed several independent risk factors associated with a given species of Candida: age, sex, ICU admission, recent surgery, underlying disease, central venous catheter, intravenous drug addiction and pre-exposure to antifungal drugs.
The crude 30-day mortality rate was higher in ICU (47.8% vs. 27.4%). In non-ICU patients, it was significantly increased in oncology patients compared to the other groups. No antifungal drug prescription and ICU admission were independent risk factors for death in all candidemic patients. Among species, Candida spp., C.glabrata (OR=0.69 CI 0.54-0.89) and C.parapsilosis (OR=0.49 CI 0.35-0.67) were associated with a lower 30-day mortality rate compared to C.albicans.
Conclusions
Despite a lack of information regarding severity of illness and concomitant bacterial infections, this database can be very useful to physicians who manage patients with candidemia, as it clearly shows that the odds of infection by a given Candida species, clinical characteristics and risk factors for death may largely vary according to the underlying malignancy and type of hospitalisation.
Article review submitted by NEXT Committee member Gennaro De Pascale and EJRC member Flavia Torrini, Department of Anaesthesiology and Intensive Care, Catholic University of the Sacred Heart, A. Gemelli Hospital, Rome, Italy.
Reference
1. Lortholary O, Renaudat C, Sitbon K, Desnos-Ollivier M, Bretagne S, Dromer F and the French Mycoses Study Group (2017) The risk and clinical outcome of candidemia depending on underlying malignancy. Intensive Care Med (2017) 43:652–662
DOI 10.1007/s00134-017-4743-y.